Vasectomy Reversal
Can a vasectomy be reversed?
Vasectomy reversal is the most cost-effective way of achieving pregnancy after a vasectomy. Whether a couples desires more children in a relationship or the desire for children in a new relationship, vasectomy reversal offers the best chance of pregnancy.
There are over 35,000 vasectomy reversals performed annually in the United States. The most common reasons for this procedure include divorce/remarriage, desire for more children in a current relationship or death of a child. Occasionally, a vasectomy reversal will be performed simply because a man has changed his mind and wishes to restore continuity of his reproductive tract or he has developed pain after his vasectomy.
Can a vasectomy be reversed?
The success rate for vasectomy reversal is greater than 95% when sperm are identified at the time of surgery. The chances of finding sperm at the time of vasectomy reversal is determined by two important factors: the time elapsed since the vasectomy and the site of the vasectomy. When the time interval between the vasectomy and the vasectomy reversal is greater than 15 years, the chances of developing a secondary epididymal obstruction is approximately 70%. Also, when the vasectomy is performed low on the vas deferens then these chances are compounded. If sperm are not identified at the time of vasectomy reversal, an epididymovasostomy will be required to reverse your vasectomy. Vasectomy reversal success with epididymovasostomy is 65-70%. Regardless of the amount of time elapsed since the vasectomy, the success rate should be constant and only dependent on the type of surgery that is required.
How is a vasectomy reversal performed?
There are two different techniques for reversing a vasectomy: vasovasostomy and epididymovasostomy. Both techniques involve bypassing the obstruction in the reproductive tract. Vasovasostomy is the preferred method of vasectomy reversal when sperm are identified in the vas deferens at the time of surgery. Epididymovasostomy is the preferred method when sperm are not seen in the vas deferens.
Back To Top
Vasovasostomy
Vasectomy reversal performed by vasovasostomy is done using an operating microscope that provides magnification 25 times the normal image size. This is important since the size of the vas deferens is about the same as a piece of spaghetti and should be sewn in two-layers to offer the highest pregnancy rates. Microscopic suture (10-0 nylon) unseen by the naked eye is used during the vasectomy reversal. It is important to use this fine suture to prevent leakage of sperm and to minimize obstruction of the lumen of the vas deferens by the suture itself.
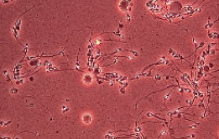
| The initial step during a vasectomy reversal is to identify whether or not there are sperm in the testicular end of the vas deferens. If sperm are identified, then a vasovasostomy can be performed successfully using microsurgical technique. If sperm are not identified then a secondary epididymal obstruction has developed and re-connecting the vas deferens at the site of vasectomy will universally be unsuccessful. This occurs 30% of the time and is dependent on several factors such as the time since your vasectomy and the site of your vasectomy. If sperm are not seen then an epididymovasostomy will be required in order to reverse the vasectomy. (see below) |
|
 |
| The next step in a vasectomy reversal is to re-approximate the ends of the vas deferens in a tension-free manner. The 10-0 Nylon suture provides a water-tight closure for the sperm to travel through the vas deferens. If larger sized suture is used, it can cause obstruction in the vasal lumen itself. |
|
 |
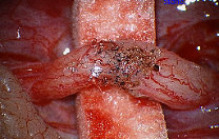
| The typical appearance of the vasal lumen after it has been precisely sewn together using 10-0 nylon suture. The suture is made of the finest non-reactive material to prevent scarring of the lumen after the surgery. |
|
 |
| An outer layer of 9-0 nylon suture is placed to reinforce the inner layer and to relieve tension from the important inner layer. Numerous interrupted sutures are placed around the outer layer ensuring a tension-free closure. |
|
 |
Back To Top
Epididymovasostomy
Epididymovasostomy is required during vasectomy reversal when there is absent sperm in the vas deferens. This signifies that a secondary epididymal obstruction has developed upstream from the vasectomy site. This situation is encountered in approximately 40% of individuals after a vasectomy. Epididymovasostomy can only be performed using a high powered operating microscope, under general anesthesia, by microsurgeons using the finest suture (10-0 nylon).
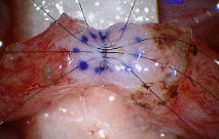
| The epididymis is opened and a single tubule is isolated to bypass the obstruction that has developed |
|
 |
| The vas deferens is then attached to the epididymis using fine sutures (9-0 nylon). This attachment brings the vas deferens into close proximity of the single epididymal tubule |
|
 |
| The single epididymal tubule is sewn to the inner lumen of the vas deferens using microscopic sutures to create a water-tight closure, similar to vasovasostomy. |
|
 |
| Additional fine sutures are placed in the outer layer of the epididymis to secure the vas deferens in place and to release tension off of the fine inner sutures. |
|
 |
| This final lower power image shows the relationship of the testis, epididymis and the bypass site after an epididymovasostomy. Sperm are made in the testis, stored in the epididymis and bypass the second obstruction through the bypass site |
|
 |
Back To Top
Who should perform my vasectomy reversal?
The leading reproductive society, ASRM, has issued practice guidelines stating that:
“Since it is seldom possible to determine pre-operatively if epididymovasostomy will be required in a man undergoing vasectomy reversal, only surgeons skilled in both epididymovasostomy and vasovasostomy should perform vasectomy reversal”
It was also stated in the practice committee guidelines that the success and pregnancy rates of men undergoing micro-surgical (24 times magnification) vasectomy reversal was much higher than in men undergoing the macro-surgical technique (2.5 times magnification, Loupe assisted).
Many urologists offer vasectomy reversal services, however El Camino Urology Medical Group offers a level of expertise held by only 1-2% of urologists nationally. Choosing our fellowship trained microsurgeon will guarantee that your surgeon meets the guidelines established by the leading reproductive society in this country.

Some urologists will try to compensate for the lack of this advanced training by offering their patients seasonal specials, vacation packages or even a money back guarantee along with their vasectomy reversal. These are gimmicks! Most respectable physicians do not ethically participate in such business practices. These specials are designed to lure unsuspecting patients into a sub-optimal situation for a vasectomy reversal. It is important to remember that the ultimate goal of your process and journey is to have a natural pregnancy after your vasectomy and not receive a free vacation or cut-rate procedure. Additionally, most of these money back guarantees are designed to only give you back a small portion of your investment and not the entire amount. Read the fine print and you will see that it really isn’t a true money back guarantee!
Instead of offering gimmicks or vacation packages, we provide the highest quality service. We are so proud of our technique and quality of vasectomy reversal that every patient receives high resolution photographs of the critical steps of their reverse vasectomy procedure. We stand behind the quality of our work by providing you proof of the high quality of the procedure with actual photos from the surgery. Without these photos, patients are left wondering what happened on the inside and oftentimes only can evaluate the quality of the incision, which has no relevance to the success of the reverse vasectomy procedure.
This is why the California Vasectomy and Reversal Center at the El Camino Medical Group is the leading vasectomy and vasectomy reversal center in Northern California. We provide our patients with the latest techniques and most sophisticated equipment when it comes to their vasectomy or reverse vasectomy procedure. We are conveniently located to all major metropolitan areas of San Jose, San Francisco, Oakland, Sacramento, Santa Cruz, Monterey, Fresno, Stockton, Santa Rosa, and Modesto. Our patients come from virtually every corner of California, Nevada, Oregon and Hawaii. Patients from Reno, Las Vegas, Portland, Bakersfield, Los Angeles, San Diego, Orange County, Riverside, Palm Springs, San Luis Obispo, Visalia and Santa Barbara have all had successful reverse vasectomy procedures performed at our center.
Back To Top
Microdot Technique Vasovasostomy:
| The Microdot method for performing vasectomy reversal is a variation of the standard multi-layer reverse vasectomy procedure.Similar 10-0 Nylon and 9-0 Nylon sutures to microsurgical vasovasostomy are used to re-approximate both layers of the vas deferens. |
|
 |
| The microdot technique allows for easy placement of the mucosal 10-0 Nylon sutures. The microdots guarantee even placement of the mucosal sutures. Re-alignment of the vas deferens is performed during the reverse vasectomy procedure to ensure patency of the lumen of the vas deferens and to prevent long-term scarring of the vasectomy reversal procedure. |
|
 |
| Once the inner luminal sutures are tied, the knots are cut precisely. Because of the very small size of the vas deferens lumen, any redundant suture material can obstruct the flow of sperm along the vas deferens. Likewise, sperm leakage outside of the lumen can cause obstruction of the vas deferens. A water tight closure of the vas deferens mucosa prevents sperm from leaking out of the vas deferens after the procedure. |
|
 |
| The outer serosal sutures are equally important in the reverse vasectomy procedure. These sutures relieve tension off of thefiner inner luminal sutures and prevent the ends of the vasdeferens from separating after the reverse vasectomy procedure. Liberal placement of these outer serosal micro-sutures needs tobe done under a microscope as well to ensure that the ends of the vas deferens are precisely approximated. |
|
 |
Back To Top
Epididymovasostmy (LIVE_Longitudina Intussuception VasoEpididymostomy Technique)
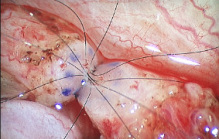
| In those cases where sperm are NOT identified in the testicular vas deferens, an epididymovasostomy or “bypass” operation is required. The typical appearance of the epididymis many years after the vasectomy procedure. |
|
 |
| A single tubule from the epididymis is isolated for the reverse vasectomy procedure. This procedure can only be accomplished under the highest magnification and the patient laying completely still under a general anesthetic. Two microsurgical 10-0 Nylon sutures are passed through the single epididymal tubule along the longitudinal axis of the epididymal tubule, prior to opening the tubule. |
|
 |
| The abdominal end of the vas deferens is re-approximated to the serosal edge of the tunic of the epididymis. The attachment of the vas deferens to the tunic of the epididymis secures the vas deferens and allows for accurate placement of the inner mucosal sutures. |
|
 |
| The microsurgical 10-0 Nylon sutures are passed through the mucosa of the vas deferens in their corresponding locations on the mucosa of the vas deferens. |
|
 |
| The 10-0 Nylon sutures are tied creating a water-tight closure between the epididymal tubule and the mucosa of the vas deferens. The single epididymal tubule is pulled (intussucepted) into the lumen of the vas deferens. |
|
 |
| Additional microsurgical sutures are placed between the tunic of the epididymis and the outer (serosal) edge of the vas deferens. The additional microsutures on the outer layer of the vas deferens relieve the tension off of the important inner luminal sutures. |
|
 |
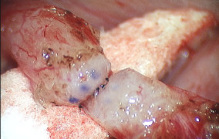
| The final appearance of the vas deferens attached to the epididymis at slightly lower magnification. The “bypass” procedure restores continuity of sperm flowing through the vas deferens when an obstruction or “blockage” is identified at some part of the epididymis. |
|
 |
Back To Top
Vasectomy Reversal Recovery, Healing and Pictures of Incisions
Patients always wonder what the recovery process is after a vasectomy reversal and what their incisions should look like after surgery. Fortunately, vasectomy reversal is not a very extensive operation regardless of which of the two surgeries are Patients always wonder what the recovery process is after a vasectomy reversal and what their incisions should look like after surgery. Fortunately, vasectomy reversal is not a very extensive operation regardless of which of the two surgeries are not getting on a plane for 3-4 hours or sitting in the car for an equal amount of time was not a problem as soon as the day after performed. The amount of time required for surgery and the need for general anesthesia should make patients think that surgery.
Your restrictions for activity after a vasectomy reversal are designed more for the actual healing process that is on-going inside the scrotum, than the actual discomfort a patient feels. The tiny microscopic sutures are all that is holding everything together after the vasectomy reversal and it is imperative that these sutures are not disrupted while allowing the surgical site to heal. There is no good medical justification to tell patients to “take it easy” for 2, 3, 4, or 6 weeks. These restrictions are quite arbitrary and usually based on a vasectomy reversal specialist’s own experience with the healing process. We feel that patients are able to resume all of their physical activities 2-3 weeks after surgery based on our surgical technique and experience.
| The typical appearance of the scrotum 1 week after vasectomy reversal surgery. The vasectomy reversal recovery shows minimal if any swelling and bruising in the scrotum. The scrotal rugae or “wrinkles” are apparent and indicative of resolution. |
|
 |
| Close inspection of the right wound reveals some scab formation on the incision line. The scab can liquefy and cause some staining on the scrotal support, gauze or underpants |
|
 |
| The left side has virtually no swelling or bruising. The incisions are both approximately one inch in length. Compared to the previous vasectomy incisions/scars the wounds are bigger. Both incisions are in the spectrum of normal healing 1 week after the vasectomy reversal. |
|
 |
|
|
|
Go Back to Services